(Actually, we narrowed it down to our favorite “Top 17” OIT Myths!)
There are so many distorted “facts” about OIT that circulate in the food allergy world. We put together a list of statements we repeatedly hear as reasons for not doing, pursuing or even learning about OIT. Yes, OIT is a medical treatment with risks. Yes, it does not work for everyone. However OIT works for the vast majority of patients with IGE-mediated food allergy in the hands of a skilled board-certified allergist.
Start here to build some understanding, then sit down for a consult with an OIT allergist and get the best information available. Also check out our FAQs/ Q&A page, our OIT Community page, and visit our Research & Learn Library for 400 articles, medical journals and tv broadcasts about OIT.
1) My child is too allergic or their allergies are “too severe” to treat with OIT: IGE >100 or Class 6.
2) My child has had too many anaphylactic reactions; our allergist agreed that no one will treat him with OIT.
3) OIT is not FDA-approved so it must not be safe.
4) It is common to have an anaphylactic reaction while doing OIT.
5) Most people have to drop out of OIT due to severe side effects.
6) If we skip an OIT dose or day, the allergy will come back, or we would need to completely start over.
7) We do not know the long-term effects of OIT and desensitization.
8) The leading food allergy researchers won’t endorse OIT as a treatment ready for private practice, so it must not be safe.
9) If OIT doesn’t work or you have to stop, the allergy might get worse, perhaps become airborne or contact reactive, or you might develop new allergies.
10) We could not do a 2-hour post-dose observation/no-exercise period with our lifestyle. My child is an athlete/active child.
11) Many / Most / A lot of OIT patients develop EoE (Eosinophilic Esophagitis) which is an allergic/immune condition with inflammation or swelling of the esophagus.
12) My child has multiple allergies; we could not do OIT for each of them and eat them all for a lifetime.
13) Everyone says we should only do OIT in a clinical trial.
14) We don’t want to do OIT because we hope our child will outgrow their allergies.
15) We do not want to do OIT because we heard children must take a food challenge before starting treatment.
16) My child is too anxious at the thought of ingesting their allergens with OIT.
17) “My allergist said…” (insert any of the points above)
1) My child is too allergic or their allergies are “too severe” to treat with OIT: IGE >100 or Class 6.
A) Everyone with real allergy has a severe allergy. There is no mild, moderate, or severe allergy. Reactions can be mild, moderate, or severe. But, there is no way to predict what kind of reaction one might have or what exposure level will trigger that reaction. Reactions are very unpredictable and variable. One reaction says little about what the next may be like. If you have a real allergy and a risk of anaphylaxis, then it is severe.
Once that is established then we act like the military–we prepare for the worst, not the most likely. I don’t care what the numbers say or how high the levels are. The numbers show the likelihood of a reaction–they do not tell severity or predict the severity of a reaction. So, we prepare for the worst case scenario. Skin test result of IgE levels are pieces to the puzzle, NOT the whole puzzle.
B) There are not patients who are too severe. See A) if you don’t get “why.”
For OIT, there is not a level threshold where numbers are “too high” or “too severe”. Why? Allergies aren’t mild or severe–reactions are. One child can have full-blown anaphylaxis with an IGE of only 2.5, yet another child might just have hives with an IGE of 100. Numbers only predict the likelihood of “a” reaction but nothing about what that reaction might be like. We have kids in OIT with very low IGE’s who have had very serious reactions before OIT.
What DOES matter in OIT is finding the “threshold of tolerance”–the microscopic amount of allergen that can be consumed without reaction. It’s that simple. Threshold of tolerance for food allergic patients has been studied since the 1990’s. These allergists can make doses that tiny that patients do not react. Then the dose is raised and the immune and digestive systems adapt and the process is repeated. It’s like allergy shots where the threshold is raised slowly, and the allergen is invisible to the body.
Dr. Sakina Bajowala explains it this way: “The only criteria for OIT are presence of an IgE-mediated food allergy and commitment to adhering to the protocol. Contraindications include uncontrolled asthma and eosinophilic esophagitis. It is also important to obtain tight control of other atopic conditions prior to beginning OIT. High food-specific IgE is not a deterrent, but may be a criterion for beginning with sublingual lead-in therapy prior to beginning OIT. There is no such thing as being “too allergic”. In fact, the patients at highest risk of anaphylaxis are the ones who have the most to gain from desensitization.”
Dr. Joel Selter concurs: “There is no such thing as being too allergic. Theoretically, any person is a good candidate for OIT.”
2) My child has had too many anaphylactic reactions; our allergist agreed that no one will treat him with OIT.
Dr. Chad Mayer: “My answer first is usually, they are who need it the most, along with those who have had anaphylactic reactions in the past. Evidence is clear that IgE level at the start of OIT does not matter. Ask any Dr. who does OIT and all of them will say there is no such thing as too allergic.”
Dr. Scott Nash: “The more severe the allergy, the greater the need for treatment.”
3) OIT is not FDA-approved so it must not be safe.
 From the literature there is overwhelming evidence that OIT will induce desensitization, meaning that the patient will be able to ingest/be exposed to the food without any reactions. From Dr. Burk’s Duke study that started in 2007, he published their findings in JACI: “This is the first double-blind, placebo-controlled study of peanut OIT as a treatment for peanut allergy. By establishing the safety and efficacy of allergen-specific desensitization, these data support the feasibility of using peanut OIT as an interventional therapy.”
From the literature there is overwhelming evidence that OIT will induce desensitization, meaning that the patient will be able to ingest/be exposed to the food without any reactions. From Dr. Burk’s Duke study that started in 2007, he published their findings in JACI: “This is the first double-blind, placebo-controlled study of peanut OIT as a treatment for peanut allergy. By establishing the safety and efficacy of allergen-specific desensitization, these data support the feasibility of using peanut OIT as an interventional therapy.”
OIT is simply a written medical protocol using food. It requires a highly skilled, trained, board-certified allergist to administer it. Being prepared and able to handle an anaphylactic reaction is what allergists do. They do it daily in food challenges in office, where doses are thousands of times larger than OIT doses.
The FDA approves commercial products for sale. They regulate the manufacturing, labeling and marketing of this product by a company who applies for FDA approval. They do not approve written medical protocols using a food that is already FDA approved. OIT as a treatment will never be FDA-approved for this reason. Read about the FDA drug approval process here:
http://www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm143534.htm
Dr. Chad Mayer explains the answer simply: “Many question if this procedure is FDA approved. OIT does not utilize a medical device or medication and therefore does not fall under the purview of the FDA and it will not approved or disapproved by the FDA.”
Dr. Richard Wasserman shares his perspective: “Regarding your question about FDA approval, the FDA does not approve treatments. They only approve drugs and devices. FDA “approval” is not required for a physician to treat a patient with OIT. In fact, the FDA will only approve a “drug” for use in desensitization by OIT. There are investigators who are studying the use “pharmaceutical quality” foods for desensitization. Most physicians currently doing OIT use off-the-shelf foods. If the FDA approves, for example, a peanut formulation for OIT, it is likely that the cost will increase dramatically because instead of paying a few dollars for a pound of peanut flour, it will become a drug. I don’t think this will help patients.”
“It has been argued publicly that more studies are needed before OIT can be offered by allergists outside of studies. Since that statement was made in a public forum, there have been more than 400,000 ER visits for food allergy and opponents say we still need to wait for more studies. OIT is a complex and demanding procedure for patients, their allergists and their allergists’ office staffs. Not every office will be equipped or willing to undertake the effort to offer this therapy. I believe that OIT should be available but I don’t believe that every allergist should offer OIT.”
 Dr. Zach Jacobs weighs in, “I’ve always tended to believe that the most effective argument against oral immunotherapy was along the lines of the cold hard economics of it. The number of food allergic kids required to do food oral immunotherapy to prevent one food allergy related death is probably quite high (meaning the number needed to treat to prevent a death would maybe be too high to justify the price of the therapy, at least on a population level). But, this economic argument that some allergists postulate no longer holds water either. Because a peanut flour pill has been fast tracked by the FDA. If one thought that the economics of OIT didn’t make sense using run-of-the-mill peanut flour that can be bought anywhere, guess what will happen when we use “pharmaceutical grade” peanut flour that the patient is prescribed? The cost of oral immunotherapy will be astronomical. Furthermore, when the peanut pill is eventually approved by the FDA, the same questions that hold many people back from offering OIT such as what’s the most effective dosing protocol, desensitization versus tolerance induction, and side effects, will all still be out there. However, since the peanut flour will suddenly be “FDA-approved” using a more regimented protocol with likely less flexibility, will there be a clamor for it? Likely so, but I guess it will be nice not to have any “stigma” associated with OIT any longer. The peanut patch will probably also be out by then and represent a nice alternative for patients that are maybe not as good OIT candidates for one reason or another.”
Dr. Zach Jacobs weighs in, “I’ve always tended to believe that the most effective argument against oral immunotherapy was along the lines of the cold hard economics of it. The number of food allergic kids required to do food oral immunotherapy to prevent one food allergy related death is probably quite high (meaning the number needed to treat to prevent a death would maybe be too high to justify the price of the therapy, at least on a population level). But, this economic argument that some allergists postulate no longer holds water either. Because a peanut flour pill has been fast tracked by the FDA. If one thought that the economics of OIT didn’t make sense using run-of-the-mill peanut flour that can be bought anywhere, guess what will happen when we use “pharmaceutical grade” peanut flour that the patient is prescribed? The cost of oral immunotherapy will be astronomical. Furthermore, when the peanut pill is eventually approved by the FDA, the same questions that hold many people back from offering OIT such as what’s the most effective dosing protocol, desensitization versus tolerance induction, and side effects, will all still be out there. However, since the peanut flour will suddenly be “FDA-approved” using a more regimented protocol with likely less flexibility, will there be a clamor for it? Likely so, but I guess it will be nice not to have any “stigma” associated with OIT any longer. The peanut patch will probably also be out by then and represent a nice alternative for patients that are maybe not as good OIT candidates for one reason or another.”
 People do not want to do OIT because the AAAAI or ACAAI or FARE have not “approved” it and it is not in current food allergy treatment practice parameters. While these are well-respected organizations and people in charge of these groups, many who are in charge of these groups have been working with potentially very profitable pharmaceutical products that basically accomplish OIT or desensitization or other unproven “treatments” like Chinese Herbs. So, there is a double standard in their recommendations.
People do not want to do OIT because the AAAAI or ACAAI or FARE have not “approved” it and it is not in current food allergy treatment practice parameters. While these are well-respected organizations and people in charge of these groups, many who are in charge of these groups have been working with potentially very profitable pharmaceutical products that basically accomplish OIT or desensitization or other unproven “treatments” like Chinese Herbs. So, there is a double standard in their recommendations.
 The stated goal for the FARE/Aimmune “OIT in a Kit” product is to get 70% of allergists to prescribe it and “with $200 million in cash we are well-capitalized to deliver on our mission,” which is to get this OIT product to reach $1.33 billion in sales (Reuters). We will very shortly see FARE announce that they have “fixed” OIT through Aimmune’s product, when the reality is that they are recycling Dr. Burk’s OIT protocol from the Duke studies conducted from 2007-2009.
The stated goal for the FARE/Aimmune “OIT in a Kit” product is to get 70% of allergists to prescribe it and “with $200 million in cash we are well-capitalized to deliver on our mission,” which is to get this OIT product to reach $1.33 billion in sales (Reuters). We will very shortly see FARE announce that they have “fixed” OIT through Aimmune’s product, when the reality is that they are recycling Dr. Burk’s OIT protocol from the Duke studies conducted from 2007-2009.
There’s no magic to 3 mg of peanut protein. It was the same in 2007, as it is now. The 2018 “FDA-approved” version of 3 mg of peanut flour is simply the same 12% defatted peanut flour milled from lightly roasted peanuts from the Golden State Peanut Co (Alpharetta, GA) with added diluents, glidants, lubricants and filling agents. (Yum! And for $5500 per year for life, versus $50 a year for Planters peanuts).
 This particular product, Aimmune’s capsule full of peanut flour plus additives, really does not add to anything what is already available for OIT. It may be marketed like it does, but it really does not. 3 mg of peanut flour is 3 mg of peanut flour, regardless of whether it was in 2007, now, or in 2018. There’s no magic in that. No rabbit coming out of a hat, transformed after 10 years of waiting.
This particular product, Aimmune’s capsule full of peanut flour plus additives, really does not add to anything what is already available for OIT. It may be marketed like it does, but it really does not. 3 mg of peanut flour is 3 mg of peanut flour, regardless of whether it was in 2007, now, or in 2018. There’s no magic in that. No rabbit coming out of a hat, transformed after 10 years of waiting.
In fact, it makes little sense that one protocol was “picked” (versus tested and published) for this product, with a goal of creating “Standardized OIT” that is safe for every peanut-allergic person. We would expect a product for the masses /general population would use a LOWER and SLOWER protocol than the “Customized OIT” the current allergists do. However, this is not the case with Aimmune. For example, the starting dose, the first dose of a series given to the patient on Day 1 under “Standardized OIT in a Kit” is 250 times HIGHER than the average dose given to Private Practice patients. We know that giving a first dose of 0.5 mg will send some patients into an anaphylactic reaction. The typical starting dose for Practice Practice OIT patients is 0.002 mg, 250 times smaller.
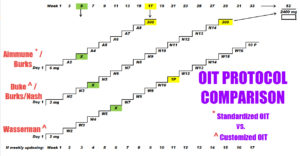 The Aimmune product continues to be higher at the typical ending dose at Day 1 of 6 mg versus 2 mg or 3 mg in Private Practice protocols, and higher and faster for each benchmark along the way. We have many patients in our OIT support groups who cannot reach the benchmarks in the “Customized OIT” protocols and have to go much slower. There will be much more risk to the public and innocent children when you match
The Aimmune product continues to be higher at the typical ending dose at Day 1 of 6 mg versus 2 mg or 3 mg in Private Practice protocols, and higher and faster for each benchmark along the way. We have many patients in our OIT support groups who cannot reach the benchmarks in the “Customized OIT” protocols and have to go much slower. There will be much more risk to the public and innocent children when you match
1) a rigid, higher and faster protocol with
2) allergists who have no background or training in OIT except what they may get from the manufacturer.
There is a deeper issue than just what is or is not available, though. Pharma-driven products may indeed have a place with some patients given their circumstances in the realm of food allergy treatment. They may provide just another option for allergists at some point.
However, when the physicians involved in these for-profit companies are also researchers at academic centers and, more importantly, occupying positions in national/international societies with influence over many–they have a conflict of interest. They do have a right to follow whatever path they want. But, those on committees that form “guidelines” should uphold a standard of being the voice of evidence-based medicine. Being involved in big-pharma products at the same time erodes the ability to maintain that objectivity. It does call into question the credibility of the recommendations from those individuals. We would hope there would be full-disclosure and conflicts of 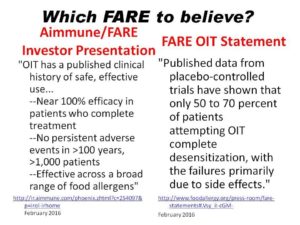 interest clearly shared. This also applies to FARE being open about being a major investor in Aimmune when they start promoting the product and FARE profits from it. Because on the one hand FARE bashes private practice OIT (so they can claim they have “fixed” OIT), yet on the other hand they are praising OIT to other investors in the Aimmune Corporate Presentation February 2016. Which FARE to believe?
interest clearly shared. This also applies to FARE being open about being a major investor in Aimmune when they start promoting the product and FARE profits from it. Because on the one hand FARE bashes private practice OIT (so they can claim they have “fixed” OIT), yet on the other hand they are praising OIT to other investors in the Aimmune Corporate Presentation February 2016. Which FARE to believe?
Patients need to be able to make more informed decisions on treatment options of a potentially life-threatening condition. We are not debating the Next-Great-Energy-Drink to hit the market. We are talking food allergy. A cynical person may feel that the research and academic physicians with strong influence over “national and international food allergy treatment guidelines”– withheld recommendations on OIT being done in clinical practice until their research was funded/completed or until their pharma-driven products were commercially available. Many in the OIT community have grown cynical since 2010, but the reason for that is because that is exactly where the evidence points 🙂. Physicians and patients should have the ability to make the best decisions possible with the best information currently available given their circumstances–unbranded and honest. That will yield real progress.
While these pharmaceutical products will help many food allergic patients, there is also a huge risk to public safety. Rather than learning and studying OIT at a deep and comprehensive level, anyone with an Rx pad will be simply follow the written instructions from Aimmune. “OIT in a Kit” has the potential to take treating a deadly food allergy right into the hands of medical professionals with no allergy training, licensing or board-certification.
4) It is common to have an anaphylactic reaction while doing OIT.
From Dr. Factor at New England Food Allergy Treatment Center: “There is a lot of misinformation being circulated about safety concerns regarding oral immunotherapy to foods or OIT. When performed by qualified allergists OIT can be both safe and effective therapy. Some people and practitioners believe OIT is not safe and there is a high rate of unsuccessful treatment. I have personally found this to be untrue. We have treated over 800 patients with peanut allergy at the New England Food Allergy Treatment Center in Connecticut. Allergic reactions during treatment are very uncommon and we have had a success rate of over 90%. My discussions with other allergists around the country who are performing OIT have had similar positive experiences. The choice by patients and parents is a personal one, and a lot of thought must going into deciding whether OIT is right for them/their child.”
 Dr. Rubina Inamdar echoes this sentiment: “In many ways it is safer than still being allergic. We haven’t needed to use Epi in our clinic during dosing or with any of our patients at home for six months. As long as parents and families can follow directions, everyone stays safe.”
Dr. Rubina Inamdar echoes this sentiment: “In many ways it is safer than still being allergic. We haven’t needed to use Epi in our clinic during dosing or with any of our patients at home for six months. As long as parents and families can follow directions, everyone stays safe.”
Dr. David Fitzhugh has found OIT empowering for parents: “Parents who have children desensitized to food allergens have less fear and anxiety about food-induced anaphylaxis…While I believe in appropriate and intelligent use of diagnostic testing and imaging when required, I have found in my training and practice that what is most important is taking the time to listen to my patients and to educate them about their conditions and the treatment plan.”
Dr. Sakina Bajowala adds perspective on the types of side effects, symptoms and reactions that could occur: “Mild reactions during food desensitization are not uncommon, and tend to be self-limited. Transient itching of the mouth and throat occur, and generally resolve within a few minutes without medication. Abdominal pain, gas, reflux, nausea, and vomiting have also occurred. These symptoms are typically managed with the following: dietary modification, antacid medication, and immunotherapy dosing adjustments. The vast majority of patients are able to resolve these symptoms with the above measures, and complete the immunotherapy protocols. Any time that a food allergen is deliberately administered to an allergic individual, the potential for a body-wide allergic reaction (anaphylaxis) exists. Although it is not typical, anaphylaxis has occurred in the context of oral immunotherapy dosing. When systemic reactions are noted, they are immediately treated with epinephrine and additional adjunctive medications as appropriate. Systemic reactions do not preclude the patient from moving forward with the protocol. In fact, all patients in our practice who have ever required epinephrine in the course of treatment have gone on to graduate from their respective desensitization programs.”
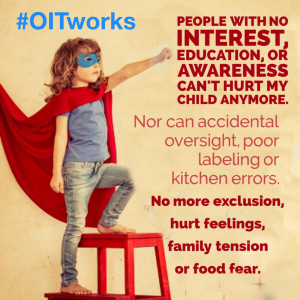
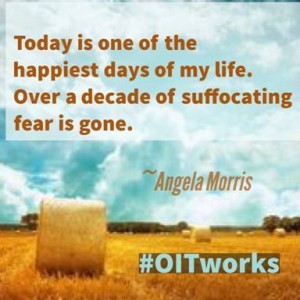
Ultimately, because post-OIT patients are possibly still allergic, though desensitized, the risk of anaphylaxis is still there. The key to understanding OIT is the tremendous upside to daily quality of life. Patients can eat what they want, not read labels, and participate in any social event and celebration without fear. “If we can normalize life by dramatically lowering the risk of a reaction when they’re exposed to the food, and give them the option to incorporate that food into their diet as part of everyday life, that’s our goal,” Dr. Wasserman says. “If we can meet that goal, we’re happy. Because that changes life.”
After treating patients for several years, Dr. Wasserman launched a small pilot study in Dallas focusing on quality of life for 31 food-allergic families who underwent OIT. He compared his findings to results from a separate survey of 352 patients who did not have OIT. The post-therapy group reported their quality of life to be about 10 times better. There are now multiple studies that confirm the enormous improvement of quality of life due to OIT.
5) Most people have to drop out of OIT due to severe side effects.
 OIT is safe. Dr. Chad Mayer: “Most patients experience mild symptoms the first day of therapy (mild hives, oral itching/burning, GI discomfort). Severe reactions are rare occurring anywhere from <1%-10% (of patients) depending on the study. Most studies the rate of anaphylaxis is 5%. This reaction rate is for the total protocol not per dose.
OIT is safe. Dr. Chad Mayer: “Most patients experience mild symptoms the first day of therapy (mild hives, oral itching/burning, GI discomfort). Severe reactions are rare occurring anywhere from <1%-10% (of patients) depending on the study. Most studies the rate of anaphylaxis is 5%. This reaction rate is for the total protocol not per dose.
Approximately 85% of patients finish the protocol, the 15% drop out rate is primarily due to inability to continue to keep to the schedule, and GI discomfort. There have been a few patients (1-2%) diagnosed with Eosinophilic Esophagitis and had to be discontinued (unknown if the patients had EoE prior or was induced by ingesting the allergen– I suspect there has been both).
The 15% drop out rate is less in protocols not following a rigid study schedule. This lower dropout rate is due to the ability to slow down the schedule when needed to allow symptoms to dissipate and be minimized.”
Dr. Wasserman says that about 15% of his patients drop out of OIT for reasons including severe reactions; stomachaches or vomiting hours after dosing; an aversion to the foods to which they are allergic; and anxiety.
Many of the OIT allergists cite success rates of 90%+ in their private practices. “Customized OIT” increases the odds of success and doses can be adjusted precisely to what the patients need, and time in between updosing can be extended to the patient. Dr. Mayer had one patient who took 7 months to get to the “typical” Day 1 dose. That would not be possible with a rigid “Standardized OIT” protocol in a kit.
6) If we skip an OIT dose or day, the allergy will come back, or we would need to completely start over.
Not true. First of all, the allergy never “leaves” so it can’t come back. When you complete OIT you are desensitized, but still allergic.
People worry about skipping a dose, but OIT doesn’t work like insulin where you need a certain amount to live or you die without it or suddenly need to start over. Nor is it like a cup that you fill and one drop over the top causes a reaction.
Instead desensitization saturates, occupies or blocks the IgE receptor sites that normally if triggered / activated by eating the allergen, would set off the anaphylactic allergic response. You need a certain amount to do this “saturation” and since they aren’t tolerant yet it needs to be replenished by eating it again and reminding the receptors it’s a friendly substance. That amount is eventually between 5-10 peanuts but once those are saturated they can eat a lot more–we say people are “fully desensitized.” Hence the final peanut challenge of 2 or 3 times more than the daily dose amount to ensure that point of “full desensitization” has been reached. We see over and over that most problems occur with getting to one peanut or so, and then it’s easy to increase as the threshold rises.
When an OIT patient eats the dose and the allergen doesn’t trigger a reaction they get the PROOF that it’s working. Daily. It’s a daily successful food challenge. There’s no question they are safe. It’s surreal to SEE your child do this daily. Liberating. Freeing.
Everyone has a tiny dose at which they don’t react to the allergen. This has been scientifically studied for decades–even from 1997– to determine safe starting doses so there is NO REACTION. Then it just builds from there. The body adapts. And once you hit a certain level, we say around 8 peanuts or a single daily serving of other allergens, you can eat unlimited. You simply don’t react.
Take a look at this 5 year study: It’s a “Sustained Unresponsiveness” (no reaction) article. They had patients stop eating peanut for a month, then 3 months. 50% achieved what is known as “sustained unresponsiveness” – or the ability to consume peanut without reacting – even three or four years after stopping OIT. Notably, the other half who did not reach sustained unresponsiveness were still able to consume a much larger amount of peanut, with less severe reactions, than they could at the study’s outset.”
Note that the half that “failed” being able to eat unlimited peanuts after being off therapy for a month were still able to eat 10-12 peanuts with the majority being able to eat 12!!! Not one child in the study ate less than 10 peanuts after totally discontinuing peanut ingestion for a month. The half that were treatment “failures” resumed OIT. So half the kids started losing “full” desensitization after being off OIT for a month but still ate 10-12 peanuts.
“Our findings suggest for the first time that in peanut-allergic patients, long-term treatment with oral immunotherapy may produce sustained benefits allowing introduction of peanut back into the diet,” said study author Dr. Brian Vickery, Assistant Professor Of Pediatrics at the University of North Carolina.”
7) We do not know the long-term effects of OIT and desensitization.
OIT has been studied for many years: the first journal article appeared in 1908. There are over 200 articles on OIT in our Research & Learn library, conducted worldwide, under many different conditions. There is no doubt OIT results in desensitization for the vast majority.
Desensitization itself has been practiced by allergists since 1911 through allergy shots. Dr. Sugerman says, “The kind of desensitization that allergists have been doing for over 100 years, i.e., allergy shots, never underwent clinical trials. And that’s the way our specialty was born.” It goes even further back: “Desensitizing isn’t new to our world. Actually Alexander the Great used to do it. He would de-sensitize his body for poison before going out to battle,” Dr. Kari Nadeau of Stanford explains.
Other forms of desensitization in wide use are for insects and venom, and drug desensitization to aspirin and life-saving antibiotics.
There is a double standard in the food allergy treatment world. “Long term” is constantly raised as an “issue”…but only for OIT. Dr. Chad Mayer explains, “We have patients that have been followed for up to and more than 10 years. We do need more studies. The “powers to be” say we need more long term studies for OIT, but say the Viaskin patch should be good to go with 2-3 years of study? There is a disconnect here (money).”
Dr. Rubina Inamdar explains the long term this way: “Many people are concerned that there is some vagueness with endpoints – i.e. what is the maintenance dose, when do people know that they are “cured” or “treated,” who can eat all the food they want and who must still avoid the food and take their maintenance doses. The dirty secret is, that we don’t know those answers for many things we do in Allergy. For example, we give patients with severe bee or wasp sting reactions allergy shots. We know we can get them better and they won’t react severely if they get stung again, but we don’t know when to stop the shots and who has a likelihood of developing an allergy back again, and when.”
 Here’s what we DO know about the long term:
Here’s what we DO know about the long term:
- Dr. Nadeau of Stanford has treated over 1000 patients with OIT, and has the longest-running study, following patients for 10 years.
- Several private practice offices have graduated hundreds of patients with success: Dr. Factor, Dr. Mendelsen and Dr. Lee over 800 patients, Dr. Baker over 500 patients, Dr. Wasserman, Dr. Silvers, Dr. Sugerman and Dr. Kamili over 300 patients.
- In a 5-year study, everyone could eat 10-12 peanuts after a month off completely stopping therapy.
- Dr. Nadeau of Stanford: has determined positive epigenetic changes at the DNA level from OIT patients
- Nadeau: Video where she says about OIT: “It’s the only known way, at the current time, to CURE someone of their allergies.”
- Children who were treated with oral immunotherapy for cows’ milk allergy showed long-term desensitisation seven years later.
- 4 year study: Egg OIT has lasting effects after stopping dosing. Long-term treatment with egg oral immunotherapy enhances sustained unresponsiveness that persists after cessation of therapy” —> 27.5% had sustained unresponsiveness after 2 years, and 50% after 4 years.
- Patients who were in early clinical trials are still doing well. Example: Bo started OIT in a 2007 clinical trial, and posted successful update 4 years after finishing the study in 2012
8) The leading food allergy researchers won’t endorse OIT as a treatment ready for private practice, so it must not be safe.
Dr. Sakina Bajowala answers: “I believe that OIT can be performed safely, but only under the supervision of a Board-Certified Allergist & Immunologist who has made a commitment to tailoring his/her practice to the treatment of food allergy. OIT is a labor-intensive procedure that requires a near-obsessive amount of attention to detail in order to minimize the risk of errors. So, to a certain extent, I do agree with those who claim that OIT is “not ready for prime time”. Not every bread and butter allergy office is set up to properly provide the level of personalized attention that OIT requires.
We do know that in qualified hands, and with the flexibility to customize protocols to the individual patient’s needs, OIT has 85-95% success rate in private practice. We know that with time on OIT maintenance, allergen-specific IgE values drop. We know that OIT can successfully reduce food allergy related anxiety and substantially improve not only safety, but also quality of life. What we are still trying to learn is how to identify those patients who are in the 5-15% of patients who are not able to tolerate OIT, whether it is due to unremitting gastrointestinal symptoms or recurrent systemic reactions. It also remains to be determined how long OIT maintenance dosing must be maintained consistently before patients can achieve “sustained unresponsiveness”, or the ability to retain tolerance to a previously allergenic food despite not consuming it regularly.
I believe the main reason why the major allergy societies do not support widespread offering of OIT in the private practice setting is the following: in order to give such blanket approval, a therapy would need to be straightforward enough that the “average” allergist could successfully perform the procedure on a routine basis. We aren’t there yet. To me, that doesn’t mean that well-qualified allergists should be prevented from helping their patients.”
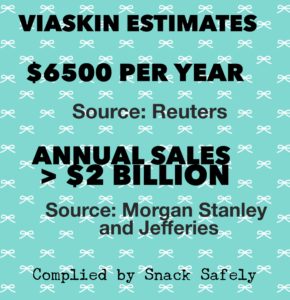 Also to note, most of the “leading food allergy researchers” are engaged in financially profiting from food allergy treatments looking for FDA approval or sold as “Chinese herbal supplements” for thousands of dollars a year right into their private company pockets. Snack Safely explains it this way: “What is the incentive for these companies and others to develop therapies? In a recent Reuters article, analysts estimated that a year’s supply of Viaskin will cost $6,500 and Aimmune’s treatment will cost $5,500. The article quotes Credit Suisse analyst Vamil Diwan estimating that (FARE’s Aimmune) AR101 could reach peak annual US sales of $1.33 billion, while analysts at Morgan Stanley and Jefferies estimate Viaskin (Patch) could reach potential for annual sales of greater than $2 billion.” Follow the money.
Also to note, most of the “leading food allergy researchers” are engaged in financially profiting from food allergy treatments looking for FDA approval or sold as “Chinese herbal supplements” for thousands of dollars a year right into their private company pockets. Snack Safely explains it this way: “What is the incentive for these companies and others to develop therapies? In a recent Reuters article, analysts estimated that a year’s supply of Viaskin will cost $6,500 and Aimmune’s treatment will cost $5,500. The article quotes Credit Suisse analyst Vamil Diwan estimating that (FARE’s Aimmune) AR101 could reach peak annual US sales of $1.33 billion, while analysts at Morgan Stanley and Jefferies estimate Viaskin (Patch) could reach potential for annual sales of greater than $2 billion.” Follow the money.
9) If OIT doesn’t work or you have to stop, the allergy might get worse, perhaps become airborne or contact reactive, or you might develop new allergies.
Question: What are implications of stopping OIT (i.e., if you dropped out or were unable to finish)? Is there a possibility of making the allergy worse?
Answer from Dr. Sakina Bajowala: “The allergen-specific IgE initially rises upon exposure to the allergen, so it is possible that a patient who discontinues therapy would have a higher food-specific IgE at the time of discontinuation that they started with at baseline. However, this number will likely fall back to baseline levels with the resumption of allergen avoidance. Additionally, it is important to recognize that although the food-specific IgE does rise at first, the food-specific IgG4 (blocking antibody) typically rises at a faster rate. Therefore, it is unlikely that a patient who needs to stop treatment will be worse off from an allergy standpoint.”
Not only is there no data to show that OIT causes more and different allergies, many of the private practice doctors have seen the opposite occur. It’s as though the immune system gets “reset”, and many patients pass food challenges for other allergens after completing OIT for one or more foods. Dr. Chad Mayer says, “I have seen something I cannot explain yet. I have a large number of patients with peanut allergy and other nuts tested positive, completed OIT for peanut and then pass all their tree nut oral challenges. I don’t know if they were false positives or treating peanut is treating the TN allergies.”
10) We could not do a 2-hour post-dose observation/no-exercise period with our lifestyle. My child is an athlete/active child.

One of the biggest “barriers” that keep people from OIT is the “Myth of the 2 Hour Rest Period.” We actually prefer the term “observation” period versus “rest”. The word “rest” implies tying them to the couch. We try not to use that word “rest period”; it has such a negative connotation. What kid would want a rest period? Naps went out in kindergarten.
“Observation period” fits because we are keeping an eye on them. After each dose, there is a 1 hour parental watch period, followed by an additional hour of no exercise. The goal is to keep the core body temperature stable as the body is digesting and metabolizing the allergen.
OIT offers a ton of flexibility in your life. We fit OIT into our lives, not our lives into OIT. During the updosing period from 4-12 months there might have to be some choices and changes as a result of doing this medical treatment. However most of us find it easy to work dosing into our plans. The actual dosing is done in 1-5 minutes; it’s eating a food. It can be done anywhere.
The post-dose guidelines we see from parents and physicians are “normal” activity–walking and moving around is fine. It’s more about not raising core body temp than heart rate. So racing up flights of stairs, wrestling, or bike riding might not be great ideas.
There are tons of “normal” things that are fine–homework, games, TV/computer, crafts, cooking, reading, carpooling, and even walking to school. If you focus on the “nots” like running or biking and reframe it as “Just don’t run!” you realize it’s a large part of the day that can fall into the 2 hour zone. Some parents have even bought Fitbit-type monitors so the kids can police themselves about heart rate and activity level.
In maintenance and even during updosing, many simply eat their dose one hour before bed. That’s quiet time anyway. Or some dose an hour before school starts, knowing that an observant teacher is watching for the second hour.
Especially at the beginning, their bodies are working HARD to metabolize and digest the peanut. This is simply a suggested precaution. What one OIT allergist has said about the no-exercise rule is that we just don’t know who needs it and who doesn’t. Many don’t, but short of dosing and putting kids on treadmills to test them exercising vigorously there is no way to know. And even with that method, there is no way to know when that might change based on illness or hormones. So it’s a flexible precaution developed because some kids have had issues.
As parents we just picture their internal engines working hard and give the body the respect it deserves! You have to realize that exercise-induced anaphylaxis with food allergies is a REAL thing and not understood well, so even without OIT it could occur.
Some doctors believe in more strict control, others are more relaxed about it. Some are strict through updosing and relax or get rid of the no-exercise precaution in maintenance. It’s an area we don’t know the answer on. The topic is an in-depth discussion to have with your doctor to assess your child’s actual risk level and what you are comfortable with. “Informed consent” in partnership with our allergist where we make the best choice for our family.
11) Many / Most / A lot of OIT patients develop EoE (Eosinophilic Esophagitis) which is an allergic/immune condition with inflammation or swelling of the esophagus.
What is EoE? From APFED: “Eosinophilic esophagitis is characterized by a large number of eosinophils and inflammation in the esophagus lining (the tube connecting the mouth to the stomach). “EoE can be driven by food allergy or intolerance: most patients who eliminate food proteins from their diet (by drinking only an amino-acid based formula) improve.”
“EoE may also be triggered by other environmental factors that researchers are beginning to understand.” These include airborne pollens; just breathing in pollen you are allergic to could trigger EoE. There is a genetic factor that is at play in some cases too. APFED: “In certain families, there may be an inherited (genetic) tendency.”
Other factors can increase eosinophils, like reflux according to APFED: “Diseases other than EoE can cause eosinophils in the esophagus including gastroesophageal reflux diseases (GERD), food allergy, and inflammatory bowel disease.” According to APFED: “People with EoE commonly have other allergic diseases such as rhinitis, asthma, and/or eczema.” More males than females are affected with EoE.
Dr. Chad Mayer: “Food allergy can lead to EoE. So if you are a person with EoE and you eat what you are allergic to, you can become symptomatic.” In other words, anyone with a food allergy is at risk of EoE. There are also people without food allergies who have EoE.
There is a risk of EoE with OIT. This study (of 15 studies) published in the US National Library of Medicine National Institutes of Health says “The overall prevalence of EoE after OIT was 2.7%” and that “EoE often resolved after OIT discontinuation.” In other words, discontinuing OIT often resolves EoE.
From perhaps the foremost authority at Cincinnati Children’s hospital: “One of the possible side effects of oral immunotherapy (OIT) is the development of an eosinophilic gastrointestinal disorder (EGID), such as eosinophilic esophagitis (EoE). This highlights the intimate connections between allergic responses that cause anaphylaxis and those involved in EGIDs. When anaphylaxis is blocked with OIT, the immune system can continue to be allergic but manifest this continued allergy via a different response (e.g. an EGID). Indeed, patients with EGID generally have IgE against specific foods but do not have concurrent anaphylaxis, further highlighting the connection. Research concerning both disorders provides novel insight on each that may not have become apparent from researching these disorders individually, emphasizing why we strongly advocate for broad research inquiry rather than a strictly focused approach and why we aim to encourage food allergy research organizations/foundations to support EGID research. To more specifically answer your question, we do not have a formal recommendation about this but wish to point out that MOST patients on OIT have not been reported to develop EGID.”
Some of the board-certified allergists have been working with patients who present with EoE after starting OIT. Dr. Richard Wasserman on OIT with EoE patients: “It is inappropriate to comment specifically on a patient that a physician has not personally evaluated so I will offer some general comments that may be helpful. I think the largest experience with EoE during OIT is that of Dr. Yitzhak Katz who has seen a pretty high incidence of EoE, proved and presumed, among his milk allergy patients. His approach has been to reduce the dose of milk until the symptoms resolve, hold at the reduced dose for a period of time (usually one to three months) and then work back up. In our experience, there appears to be a predictable syndrome in some OIT patients. There is vomiting 4-8 hours after dosing. These patients uniformly have an elevation of blood eosinophil compared to pre-treatment baseline. Based on Dr. Katz’s experience we reduce the dose until the symptoms resolve and hold at the lower dose until the blood eosinophil count returns to baseline. This usually takes one to three months but sometimes takes longer. Almost all of our patients are able to continue on.”
12) My child has multiple allergies; we could not do OIT for each of them and eat them all for a lifetime.
Multi-allergen OIT (mOIT) is on the horizon and many of the allergists are implementing it in their practices. Some group certain foods together like milk and egg, others do multiple tree nuts together for example, and others allow “up to 3” or “up to 5” to be combined at once.
We have patients in our OIT Facebook support groups who have desensitized 20+ food allergens through OIT. Some alternate the foods throughout the week or stay at a lower dose to provide “bite proof” protection (from accidental ingestion) and a lower quantity of food to be eaten regularly in maintenance.
“If something is not impossible, then there must be a way to do it.”
~Sir Winton.
Use of the drug Xolair is being studied to allow multiple foods to be more easily combined in mOIT therapy. While Xolair has some risks of its own, studies appear promising for people with multiple food allergies to be able to desensitize to more allergens at once.
 As for a lifetime? There is less evidence on long term tolerance (basically is this a cure?). Studies are still ongoing on if therapy will induce long term tolerance where daily doses will no longer need to be given. We know from a number of studies that after a period of time (studies have varied this length of therapy) that daily dosing can be discontinued and for a month or two the patient remained desensitized. All of these trials then put the patient back onto daily dosing schedule. When will you be able to stop the daily dosing at home? That question cannot be answered at this time. It will be for at least 3-5 years, and most likely longer or a lifetime for some patients.
As for a lifetime? There is less evidence on long term tolerance (basically is this a cure?). Studies are still ongoing on if therapy will induce long term tolerance where daily doses will no longer need to be given. We know from a number of studies that after a period of time (studies have varied this length of therapy) that daily dosing can be discontinued and for a month or two the patient remained desensitized. All of these trials then put the patient back onto daily dosing schedule. When will you be able to stop the daily dosing at home? That question cannot be answered at this time. It will be for at least 3-5 years, and most likely longer or a lifetime for some patients.
Dr. Sakina Bajowala explains it this way: “Desensitization occurs quickly, and refers to the process of saturating the IgE receptors and preventing cross-linking of IgE molecules on the surface of mast cells. Induction of tolerance takes longer, and refers to the long-term protection (even when maintenance dosing is discontinued). The time to achieve true tolerance is likely different for each patient depending on starting IgE values, treated food, and quantity of maintenance dose.”
“The majority of patients undergoing OIT are able to reach maintenance doses, and continue them long-term. Depending on the maintenance dose, free inclusion into the diet may also be a goal. My expectations for my patients is that the longer they continue maintenance dosing, the more likely it is that the “retraining” of the immune system will be cemented into immunologic memory, eventually leading to sustained unresponsiveness or tolerance. Side effects are possible at any stage of treatment, especially in the context of co-seasonal environmental allergen exposure, hormonal changes, rapid cardiovascular circulation or increased core body temperature. However, as allergen-specific IgE continues to fall, hopefully to undetectable levels, the ongoing risks of systemic reactions should also be decreased. I cannot over-emphasize the importance of maintaining an overall healthy lifestyle as it pertains to optimizing the benefits of food immunotherapy in the long-term. Avoiding vitamin D insufficiency, maintaining a proper balance of gut flora, limiting antibiotic use, and consuming a colorful diet heavy on fresh produce and herbs/spices which promote healthy digestion are all key.”
Dr. Richard Wasserman: “We really don’t know if dosing is for a lifetime. It appears that some children develop sustained unresponsiveness with profound reductions (>98%) of the food specific IgE. These children don’t have to dose daily. At this point, it seems that most OIT patient will need to dose indefinitely. The allergic response is still only partially understood. We don’t know why some people develop food allergy nor why some respond to OIT better than others.”
The most exciting lifetime news is that research in Dr. Nadeau’s Stanford lab has found that treating allergies with OIT actually changes the genes by epigenetics (a chemical modification of the genes that does not affect the actual DNA sequence), so desensitizing children may reduce the likelihood that they will pass on the disease to their children. She and her team now have an 10-year study of OIT — the longest record in the United States — in which they found that everyone who was compliant with the treatment and continued to eat the foods has kept their allergies from returning. Dr. Nadeau says, “It’s the only known way, at the current time, to cure someone of their allergies.”
13) Everyone says we should only do OIT in a clinical trial.
“The person who says it cannot be done should stop interrupting the person doing it.”
~Chinese proverb
The standard advice food allergy families get, “Only do OIT in a clinical trial” doesn’t make sense. The actual desensitization process between private practice and trials is similar: home dosing is 93% of it and supervised updoses 7% of the time with an allergist and staff member trained to handle any reactions that occur. Being prepared and able to handle an anaphylactic reaction is what allergists do. They do it daily in food challenges in office, where doses are thousands of times larger than OIT doses. Several of the OIT doctors actually started their careers in research and came out into private practice. Many have associated Clinical Research businesses in addition to their private practice and conduct research in multiple areas of allergy and immunology.
OIT has been done in private practice for nearly a decade. There are 70+ doctors in 2016 offering OIT in their offices. All the OIT allergists are board-certified allergists with full practices. For almost all, OIT is just a small part of their overall practice. 84% of OIT patients have insurance coverage for their treatment.
 Dr. Richard Wasserman, PhD and MD, is a pioneer and creator of one of the most widely-used OIT protocols. He states: “Clinical trials are really important and we depend on them to provide us with more rigorous information. But children are suffering now. I don’t think every ‘i’ must be dotted and every ‘t’ crossed before you help people.”
Dr. Richard Wasserman, PhD and MD, is a pioneer and creator of one of the most widely-used OIT protocols. He states: “Clinical trials are really important and we depend on them to provide us with more rigorous information. But children are suffering now. I don’t think every ‘i’ must be dotted and every ‘t’ crossed before you help people.”
Dr. Zach Jacobs: “OIT works. I don’t think that any of the arguments that contend for more research prior to it being offered in practice, especially in regards to peanut, hold any water. Research should continue, don’t get me wrong. Research on allergy shots for environmental allergies continues even while subcutaneous allergen immunotherapy is widely practiced in the community. The research is there to fine-tune the practice and answer questions as they arise. But fundamentally, I believe that oral immunotherapy to foods is safe and effective.”
As for doing OIT only in clinical trials, there are a number of advantages to doing OIT in the office of a board-certified allergist. OIT is different than most therapies being studied–usually to “get” the treatment or medicine the only way is to enroll in a trial or study. Here you can call a private doctor who specializes in OIT and perhaps start this month and go at your own pace, with “customized” OIT based on your threshold. We find that 84% of patients have had insurance coverage in the last 2 years, up from only 43%> 2 years ago.
Researchers typically don’t get funding to keep studying the same thing, so the OIT studies usually have a twist or mission or specific research question other than “does it work?” So there are very specific criteria to “qualify” for a study, and often long waiting lists.
Often in food allergy trials if you end up in the placebo leg, at the end (months or years) they allow you to switch into the active leg. You do get treated eventually, and that’s the “carrot” that they have to offer. But you can spend months or a year getting no treatment if you are in the control leg.
For people who can’t afford private practice or don’t have insurance coverage, trials are a GREAT option. Or if you didn’t have an OIT doctor nearby and only a trial then it makes sense to jump at it. Or if a trial meets YOUR specialized need better like on a 12-month old child or for multiple allergens at once.
While trials have some flexibility built in, by nature they are set in stone for dosing and timing to maintain uniformity for data collection. If you look in our Facebook OIT support groups at any given time you’ll see posts of people who needed adjustments to dose or timing, which is what a private doctor can get you.
Want to take a month off from updosing due to sickness or vacation? Back down on a dose for tummy troubles and hold for a month, or two? No problem in private practice. You can do that a bit in trials but not too much, they have clear benchmarks participants must meet or be removed from the study.
 People obviously do “fail out” of trials where it would be a mutual choice to stop OIT treatment with a private doctor. When you try and updose to a set schedule it doesn’t always work. We had one mom in our Facebook support group whose child threw up daily for 5 weeks straight trying to meet the clinical trial requirements to get to 300 mg by a certain date. That wouldn’t happen with your own doctor; your pace and dose would have been slowed down at the first sign of trouble.
People obviously do “fail out” of trials where it would be a mutual choice to stop OIT treatment with a private doctor. When you try and updose to a set schedule it doesn’t always work. We had one mom in our Facebook support group whose child threw up daily for 5 weeks straight trying to meet the clinical trial requirements to get to 300 mg by a certain date. That wouldn’t happen with your own doctor; your pace and dose would have been slowed down at the first sign of trouble.
Clinical trials absolutely have more monitoring and bloodwork requirements because they need it as a benchmark. Blood, skin and a food challenge at the beginning and end of treatment, and sometimes throughout. Trials also always require an oral food challenge before you start because they need the benchmark to measure progress. In private practice the only thing that matters is tolerating the dose and the initial doses are already determined in the protocol, and chosen through science with highs odds there will NOT be a reaction. It’s the opposite of a required food challenge in a clinical trial.
One last consideration is important–what is the long term care plan? We are with our OIT doctors for life. They are constantly studying OIT and sharing with each other what works. What happens when the trial is over? Often the researchers are researchers and go on to do something else when the trial is over. Yes, they may still be available to you, but are they dedicated to treating lots of patients with OIT and developing expertise?
14) We don’t want to do OIT because we hope our child will outgrow their allergies.
 That is an excellent reason to delay OIT! No allergist wants a child to do a lifelong treatment if they do not have to. This is another, less-cited reason for doctors preferring to wait to do OIT until the child is 4 or 5 years old and trends can be accurately tracked and evaluated.
That is an excellent reason to delay OIT! No allergist wants a child to do a lifelong treatment if they do not have to. This is another, less-cited reason for doctors preferring to wait to do OIT until the child is 4 or 5 years old and trends can be accurately tracked and evaluated.
From Dr. Wasserman, Dr. Sugerman, Dr. Silvers and Dr. Kamili:
“Peanut allergy is one of the most common food allergies and tends to be lifelong; only about 20 percent of children are fortunate enough to outgrow it. An even lower number of those with tree nut allergies —14 percent —will lose that allergy. And only 4 to 5 percent of children with a fish or crustacean (shellfish) allergy will go on to be able to eat those foods without a reaction later in life.”
“A study published in 2013 in the Annals of Allergy, Asthma and Clinical Immunology revealed these findings:
- Only 26.6% of the children in the study outgrew their allergies, at an average age of 5.4 years old.
- Children who were allergic to milk, egg, or soy were most likely to outgrow their allergies. The likelihood of outgrowing shellfish, tree nut, and peanut allergies was significantly lower.
- The earlier a child’s first reaction, the more likely that child was to outgrow the allergy.
- Other factors that contributed to outgrowing an allergy included having a history of only mild to moderate reactions, being allergic to only one food, and having eczema as the only symptom. Conversely, children with severe symptoms (trouble breathing, swelling, and anaphylaxis) and multiple food allergies were less likely to achieve tolerance.
- Black children were less likely to outgrow their allergy than white children.
- Boys were more likely to outgrow their allergy than girls.”
http://www.dallasallergy.net/outgrowing-food-allergies-odds/
15) We do not want to do OIT because we heard children must take a food challenge before starting treatment.
 Incorrect. When doing OIT with a board-certified allergist in their private practice office there is no food challenge required to start treatment. That is different than an OIT clinical trial.
Incorrect. When doing OIT with a board-certified allergist in their private practice office there is no food challenge required to start treatment. That is different than an OIT clinical trial.
Trials and studies also always require an oral food challenge before you start. The goal is to elicit a measurable reaction because they need the benchmark to measure progress after treatment. Starting OIT in private practice is the opposite: we do not want or need to get a reaction; in fact the goal is NOT to have a reaction.
In private practice the only thing that matters is tolerating the dose and the initial doses are already determined in the protocol, and chosen through science with high odds there will NOT be a reaction. It’s the opposite outcome: the dose is invisible to the body and there is no reaction.
Starting OIT doses have been studied since the late 1990’s to determine safe, non-reaction levels. The dosing escalation protocols typically don’t shift patient to patient–they are often uniform. Because for the vast majority the established doses work since they are lower than the patient’s “threshold”.
However, the allergist can quite easily customize the dose to the patient and their unique threshold. They start with doses that are hundreds of times smaller than what they think can be tolerated by the end of Day 1.
So why would a private practice OIT doctor deviate from that and do a food challenge before OIT? Well first, no doctor wants a child to do lifelong OIT if it is a false positive or a child is outgrowing on their own. This is where the reaction and patient history and all historical lab values are factored in with the doctor’s experience. Sometimes a challenge is given with the high expectation the patient will pass it. So it’s not a challenge to find a starting dose–but to avoid OIT and be FREE from a food allergy.
Sometimes, the doctor might suspect a higher threshold and offer a challenge in order to start at a higher dose. This doesn’t happen a lot, but it can happen. Why start at 2 mg if you could tolerate 50mg? That’s an individual choice–informed consent–between a doctor and patient.
There is also an optional “final challenge” at the end of treatment for patients who become “fully desensitized”, essentially to a full serving of the allergen. The final challenge is given that is 2 or 3 times higher than that daily dose. This PROVES the patient is fully desensitized, and in theory could eat unlimited amounts of the allergen.
 Dr. Sakina Bajowala explains food challenges before OIT this way, “Depending on the clinical history and results of skin/laboratory testing, a supervised oral challenge may be recommended prior to pursuing OIT. These challenges are designed to identify those patients who actually tolerate the foods to which they are sensitized. We have, on occasion, discovered that patients who were previously advised to avoid peanuts on the basis of a positive skin test are actually able to tolerate an entire serving of peanut butter (~20 peanuts) without experiencing an adverse reaction. These patients do not require desensitization. We do not generally perform food challenges in patients with a clear clinical history of food-associated reaction.”
Dr. Sakina Bajowala explains food challenges before OIT this way, “Depending on the clinical history and results of skin/laboratory testing, a supervised oral challenge may be recommended prior to pursuing OIT. These challenges are designed to identify those patients who actually tolerate the foods to which they are sensitized. We have, on occasion, discovered that patients who were previously advised to avoid peanuts on the basis of a positive skin test are actually able to tolerate an entire serving of peanut butter (~20 peanuts) without experiencing an adverse reaction. These patients do not require desensitization. We do not generally perform food challenges in patients with a clear clinical history of food-associated reaction.”
Dr. Zach Jacobs says, “Prior to my OIT life, the main reason to do a food challenge was to see if a child had outgrown their food allergy. Now, it is just as common for me to perform a food challenge to confirm the food allergy prior to undergoing such a time intensive process. As exciting as it is to see a food allergic kid progress through oral immunotherapy and tackle the food head on, it is just as exciting and rewarding to have a child pass a food challenge to something that they previously thought they were allergic to–and leave the clinic that day with complete and total freedom from that food’s effect on their life. I have seen a kid with a peanut IgE of 12 and ara h2 IgE of 5 pass his challenge with flying colors. I have also seen a kid with a walnut IgE of 0.6 fail a challenge on the first dose.”
16) My child is too anxious at the thought of ingesting their allergens with OIT.
 Dr. Sakina Bajowala addresses anxiety: “It is understandable that a child (and his/her parents) would have a certain level of anxiety when faced with the prospect of deliberately ingesting a food allergen. One of the best ways to ease the anxiety associated with this process is to speak with other families who have already completed desensitization. We have many wonderful families who have offered their time to speak with prospective patients about food desensitization. It will not be difficult to find a peer that your child can talk to as well. At the end of the day, you cannot force a child to consume their allergen against their will. It would be entirely too traumatic, from a trust perspective. That is why we work to alleviate anxiety and obtain full buy-in from pediatric patients before beginning therapy.”
Dr. Sakina Bajowala addresses anxiety: “It is understandable that a child (and his/her parents) would have a certain level of anxiety when faced with the prospect of deliberately ingesting a food allergen. One of the best ways to ease the anxiety associated with this process is to speak with other families who have already completed desensitization. We have many wonderful families who have offered their time to speak with prospective patients about food desensitization. It will not be difficult to find a peer that your child can talk to as well. At the end of the day, you cannot force a child to consume their allergen against their will. It would be entirely too traumatic, from a trust perspective. That is why we work to alleviate anxiety and obtain full buy-in from pediatric patients before beginning therapy.”
Tips from veteran OIT parents:
Parents need to understand the science behind it and how OIT works. Luckily there are hundreds of articles and clinical studies to read, and videos to watch. It’s actually overwhelming how much is available.
We see that those who choose OIT are those experiencing “pain” of some sort: whether it’s exclusion/missing out, tired of being different, anxiety over food, family issues, or having terrifying anaphylactic reactions. The “payoff” becomes so attractive that doing the work and taking the risk that OIT won’t work becomes an attractive option. It’s the famous “pleasure/pain principle”.
So, for a kid who doesn’t want to do OIT look at their “pain.” If the FA life isn’t causing he them any–why is that? It may just be a laid-back kid who takes it in stride.
What we see more of is that it’s the PARENTS who have all the stress and work really hard to protect their kids from feeling different (and make ourselves crazy in the process). Which is awesome if you don’t want to pursue treatment. But if you want to do treatment, perhaps your child isn’t feeling “pain” so there is no discomfort and no payoff that they can see. Younger kids are still pretty confident and can feel totally safe because YOU are going nuts to accommodate them.
So if you want your child to experience “real life”, then focus on not overcompensating for the allergy. Safe yes, but perhaps not always included or accommodated as much as you have been. Because it’s these kids, who never have reactions and aren’t excluded from anything because Mom is there to make it ok, these are the kids who feel invincible as teens. There’s no “pain” from the allergy so they start sneaking food and not carrying Epi. And we read their tragic stories in the news.
For older kids and teens, along with the above, you make doing OIT their choice. They MUST buy in. It’s their life and their body. But understand their valid fear and total ignorance of how this works. What has worked well for parents is to assure them “IF AND WHEN” is their choice. But, here’s the catch: they must explore OIT and learn about it. Sort of like a science project. This is a life skill you can give them about how to manage their health and make tough decisions. Require them to learn the science behind OIT. How it works. Thresholds of tolerance. Read the articles and studies. Watch the other kids’ videos and postings. Then develop a list of questions, fears and concerns and go for a consult with an OIT doctor. They are used to terror.
Then, after they complete all this, your child can make the INFORMED DECISION if they want to do OIT or not. We have seen this work time and time again. It’s parenting and empowering at its finest, to teach them to research and ask questions of a doctor.
OIT won’t be the right choice for every family. However, it is a completely normal response to start, for a child to say “no way.” We guess that 98% of the kids who have done OIT weren’t at all excited by the prospect of eating their allergen.
But it is our job as the adult/parent to provide information, counseling (which many kids need because of their food allergies), and ultimately to make the choice in care for our children. If your child needed a new kidney but was afraid of surgery no one would say, “I like to let them decide.” This is equally life saving, but clearly a choice that each family makes for themselves.
17) “My allergist said…” (insert any of the points above)
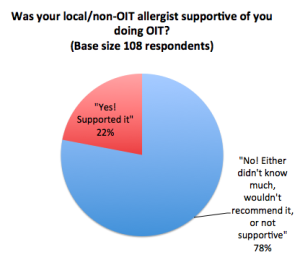
78% of OIT parents did not get support or correct knowledge from their local allergist. They had to get correct information from an OIT allergist to make the choice to do OIT.
Most doctors who advise parents to choose “Strict Avoidance” don’t fully grasp how contaminated our food system is. Every week we see on Facebook support groups, “My child had a reaction and I only fed them safe food.” Allergists don’t see the reality of 200,000 ER visits and millions more that don’t go to the ER each year. So OIT “looks” riskier because they think the odds of anaphylaxis are near zero with “Strict Avoidance.” If it really was, if we really could keep them safe easily without treating them we would certainly do that. Those of us who have done OIT don’t believe strict avoidance was a good strategy for us.
 The simple fact is that “Strict Avoidance” is an epic fail. The numbers are staggering with 200,000 ER visits, 200 deaths and millions of reactions that don’t go to the ER every year. Millions.
The simple fact is that “Strict Avoidance” is an epic fail. The numbers are staggering with 200,000 ER visits, 200 deaths and millions of reactions that don’t go to the ER every year. Millions.
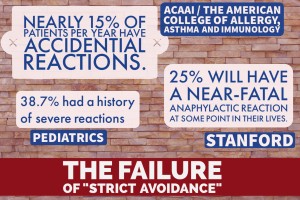
Without OIT, The American College of Allergy, Asthma and Immunology (ACAAI) says nearly 15% of patients per year have accidental reactions. Stanford says approximately 25% will have a near-fatal anaphylactic reaction at some point in their lives. Among children with food allergy, 38.7% had a history of severe reactions according to Pediatrics journal. Those are REAL odds, and in addition you have to live on hyperalert, deal with exclusion and social/family/school stress and food fear.
And truthfully, most doctors can’t have insight to the in fear, exclusion and stress parents of food allergic children grapple with. The always-on-edge worry. Every bite of food we watch them eat. Our children’s faces when they are left out once again.
Doctors are also pretty conservative. And today’s doctors don’t “doctor” much–they wait for someone to tell them what is approved and what is safe. Journals, annual meetings and drug reps are their sources. No one is out there telling them how successful OIT is in private practice. So it makes perfect sense that looking at it from their perspective, why risk anaphylaxis? “Strict avoidance works great! Just avoid it!!”
We know it’s just not that easy. You have to compare the risks and benefits of BOTH choices. Strict Avoidance vs. OIT.
Talk to an allergist who does OIT. . . Listening to scare tactics or misinformation from our doctors happened to 78% of us in OIT. We found new doctors who are actually doing it and know what they are doing. That’s what people get second and third opinions, especially from doctors who have success in doing specialized treatments that require special training. Getting a surgical opinion from a non-surgeon doesn’t make sense, does it?
The bottom line:
Now Click on the map and find an OIT allergist near you!
Various authors.
Research & Learn Library: over 400 news stories, media coverage and medical journal articles.
FAQs / Q&A: answers to common questions about OIT